The OPTIONS Consortium objective is to develop a streamlined, adaptable product delivery platform for current and future ARV-based HIV prevention options, with a particular focus on women.
Project priorities selected for year two. OPTIONS identified two priorities for project year two: (a) support country efforts to identify and reach at-risk adolescent girls and young women (AGYW) for oral PrEP and (b) develop and provide tools, resources, and targeted technical assistance to OPTIONS core countries and others considering oral PrEP implementation. Some of the anticipated OPTIONS activities planned for the coming year include development of oral PrEP rollout scenarios, cost and impact modeling for oral PrEP and dapivirine ring, investment case for dapivirine ring, market shaping communications, oral PrEP provider training materials, provider surveys (knowledge, attitudes, practices, and beliefs), and ongoing support for national PrEP technical working groups (TWGs) in Kenya, South Africa, and Zimbabwe.
Rollout scenario analyses underway. OPTIONS is developing analyses that will help decision-makers assess the potential impact of introducing oral PrEP on HIV incidence and “readiness” for introducing oral PrEP under different scenarios (e.g., in certain counties or for specific populations). The rollout scenarios will be tailored to the needs of OPTIONS core countries (Kenya, South Africa, and Zimbabwe) and will focus on how to deploy resources by exploring questions such as:
- In which sub-national regions (e.g., districts, counties) does oral PrEP availability have the highest potential for impact on HIV incidence?
- What do we know about target populations for oral PrEP and how to reach them?
- What assets exist in these regions to support oral PrEP rollout? For example, what healthcare facilities are accessible?
- What NGO programs exist that could support rollout for target populations?
- How much existing knowledge and demand exists for analogous health products and services like HIV testing or contraception?
- What are the cost implications of making oral PrEP available to AGYW in these districts? (will not be incorporated until late 2017)
The analyses will be developed by FSG in close collaboration with OPTIONS country partners (LVCT Health, Pangaea Global AIDS, and Wits RHI) with input from OPTIONS modelers Avenir Health and the London School of Hygiene and Tropical Medicine (LSHTM). Initial drafts of the analyses will be available in January 2017 and will be refined periodically as new information becomes available.
Country partners continue engaging with national TWGs. Pangaea Global AIDS drafted the oral PrEP chapter of Zimbabwe’s national ARV consolidated guidelines, as well as an oral PrEP fact sheet that will be distributed with the guidelines in the coming months. In South Africa, some of the information, education, and communication (IEC) materials from the oral PrEP launch have been updated based on NDOH and partner feedback and are available on the MPii Tools and Resources and South Africa Close-Up pages on PrEPWatch. In Kenya, LVCT Health is participating in the NASCOP PrEP TWG meetings, as well as in several of the TWG subcommittees.
Resources and tools being developed to support PrEP rollout beyond core countries. The OPTIONS Consortium has identified several priority questions raised through the PrEP TWGs in Kenya, South Africa, and Zimbabwe and with input from other countries seeking to introduce oral PrEP. These questions highlight areas where tools and resources may help support oral PrEP rollout in other countries. To help fill this gap, the team is working on developing resources to inform oral PrEP rollout in non-OPTIONS countries based on the project’s experience within its three core countries. The first questions that will be addressed are “How do countries start the process of oral PrEP introduction?” and “What do we know about implementing oral PrEP to date from demonstration projects?” Stay tuned!
Wits RHI has been collaborating with the Southern African HIV Clinicians Society (SAHCS) and partners in the development of an oral PrEP provider training package. This resulted in two packages – the first was adapted for the NDoH rollout of oral PrEP for sex workers. The second, a more generic package, was used for a national training program in nine provinces for SAHCS members during the year. Out of this process, the need for a more flexible package was identified to cater to different healthcare provider audiences, in both the public and private sectors, with clinical, programmatic, communication, and sensitization modules. The generic package will be used in South Africa and can be adapted for other countries. Wits RHI is providing technical support and oversight for this revised package.
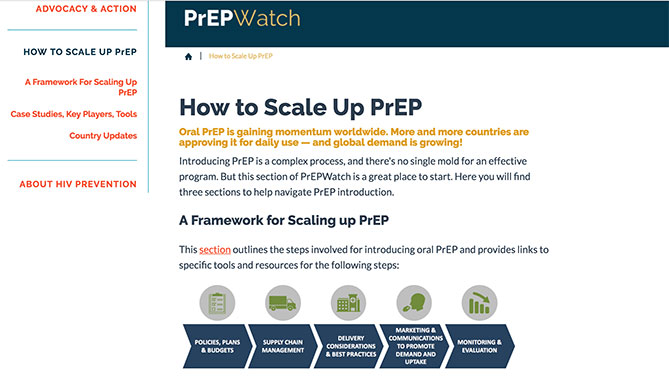
Another resource added to PrEPWatch. In addition to the new “How to Scale Up PrEP” section, the South Africa Value Chain Situation Analysis, which tracks the current state of oral PrEP rollout in the country, is now available on the MPii Tools and Resources and South Africa Close-Up pages on PrEPWatch.